Medicare Moves to Cover Costly Cell Therapies
08 Agosto 2019 - 3:38AM
Dow Jones News
By Jonathan D. Rockoff
Medicare and Medicaid will cover an expensive new kind of cancer
drug and related services, though the federal government insurance
programs won't pay 100% of the costs, which can approach $1 million
a patient.
The move, announced Wednesday by the Centers for Medicare and
Medicaid Services, could pave the way for more patients to get the
cancer drugs, known as CAR-T treatments because hospitals will know
they can get payments covering some if not all of the costs.
"We're taking action to make sure we're modernizing the program
to provide access to the latest therapies," CMS Administrator Seema
Verma said in a conference call with reporters.
Under the new move, known as a national coverage decision,
hospitals will know they can get Medicare and Medicaid
reimbursement for at least 65% of the costs of the drug and related
treatment. Hospitals can ask for even more reimbursement if they
encounter additional costs.
Hospitals will have to wait, however, for CMS to figure out the
full cost of CAR-T treatment that it will pay and to issue a
billing code for the care.
CAR-T is a new kind of drug, which takes a patient's own cells
and engineers them to fight cancers. So far, the Food and Drug
Administration has approved two: Kymriah from Novartis AG and
Yescarta from Gilead Sciences Inc. for certain lymphomas and
leukemias.
The treatments provide new options for the cancer patients. Yet
their use has been limited, in part because hospitals aren't always
sure they could get reimbursed for both the cost of the drugs and
the lengthy hospital stays for side effects and other care that are
often required.
The problem was that health-insurance payments aren't structured
for treatments like a CAR-T, which trigger not just the price of
the drug itself but related care costs that can reach hundreds of
thousands of dollars. Novartis listed Kymriah for $475,000, while
Gilead priced Yescarta at $373,000.
Until the latest move, hospitals weren't sure they could get
paid beyond the cost of the drugs and if they did, how much the
payment would be.
CMS said last week that it would pay at least 65% of a
hospital's costs, but the announcement left coverage decisions to
private regional contractors hired by the agency to administer
claims. The contractors will grant reimbursement so long as certain
criteria are satisfied, such as the hospital gives the drug for a
use that the FDA approved or that is outlined in medical guidelines
approved by CMS.
Dr. Verma described CMS's newest move as an interim step, while
the agency gathers more information about how much CAR-T treatment
costs in order to develop a payment rate and accompanying billing
code.
"There will be more to come from the agency on CAR-T," Dr. Verma
said. She added that the agency still faces the issue of how to pay
for such expensive new treatments over the long term.
Write to Jonathan D. Rockoff at Jonathan.Rockoff@wsj.com
(END) Dow Jones Newswires
August 07, 2019 21:23 ET (01:23 GMT)
Copyright (c) 2019 Dow Jones & Company, Inc.
Grafico Azioni Novartis (NYSE:NVS)
Storico
Da Mar 2024 a Apr 2024
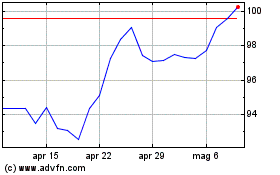
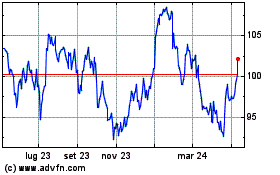
Grafico Azioni Novartis (NYSE:NVS)
Storico
Da Apr 2023 a Apr 2024