By Anna Wilde Mathews
Some of the largest health insurers are capitalizing on recent
massive deals by steering patients toward clinics they now own,
controlling both delivery and payment for health care.
The trend creates worries for rival doctor groups and hospital
companies that have invested deeply in buying up physician
practices, which now increasingly compete against offerings from
insurers.
UnitedHealth Group Inc.'s insurance unit is offering a plan in
the Los Angeles area built around doctors who work for its Optum
arm, which has acquired a sprawling network of doctor practices,
surgery centers and urgent-care clinics. The company says it is
working to offer similar designs in other markets, though they
might also involve non-Optum doctors.
"Health care has got to be more seamless and more integrated,"
said Rob Falkenberg, chief executive of UnitedHealthcare's
California operation.
At Aetna Inc., which was acquired by CVS Health Corp., many
insurance plans this year have dropped co-payments for members if
they go to the drugstore chain's MinuteClinics. Going to other
retail clinics would generally require a co-pay. CVS says the free
MinuteClinic visits are to benefit Aetna members, and not aimed at
bolstering the drugstore chain's customer traffic.
Blue Cross & Blue Shield of Texas launched a plan this year
that includes free primary-care visits at clinics it recently
opened with a partner company in the Houston and Dallas areas. It
priced the coverage 12% to 18% below a different product it offers
statewide. The new plan includes some independent doctors and
clinics, but members who use them would have a co-pay for
primary-care visits.
Blue Cross of Texas expects the clinics will lower costs by
reducing use of emergency rooms and improving preventive care, said
Shara McClure, a senior vice president at the Texas insurer, a unit
of Health Care Service Corp.
Generally, plans built around a health insurer's own clinics
include smaller networks with more limited choices of doctors and
hospitals. That can lower premiums -- but the insurers also can
benefit because they keep revenue inside their own holdings rather
than paying outside companies for the care of their members.
"It's very worrisome for hospitals," said Chas Roades, a
health-care consultant. "Suddenly, the plan you're relying on for
payment is also competing with you at the front end of the delivery
system."
Hospitals' biggest concern may be the power that primary-care
doctors have over where their patients go for care such as imaging
scans and specialist procedures. Hospitals rely on doctors to
direct patients to them for such services -- one reason they have
bought up physician practices. Insurer-owned clinics might refer
patients away from certain hospital systems, cutting off important
revenue.
Referrals are a focus for clinics owned by a joint venture
involving Florida Blue's corporate parent, said Chuck Divita,
executive vice president at the Florida insurer. Florida Blue
offers plans largely built around primary care at clinics where
members don't have a co-pay for those visits. Mr. Divita said the
clinics would aim to refer patients to specialists and other
health-care providers that deliver the best outcomes.
Some companies have offered both insurance and health care,
including Kaiser Permanente, the big California-based health plan
that has its own network of hospitals and doctors. Insurer Highmark
Health took over a Pittsburgh-area hospital system in 2013. And
some hospital operators, such as Virginia's Sentara Healthcare,
have sold their own health plans.
But deals like the CVS-Aetna merger and Optum's provider
acquisitions have created integrated health-care giants on a new
scale. Humana Inc. recently joined with a private-equity firm to
expand its primary-care clinics serving Medicare members, and it
has taken on home-health and hospice assets.
Buying up health-care providers like clinics can create
complications for insurers. Typically, they won't own enough to
offer every health-care service, so they have to keep working with
outside doctors and hospitals. And the health-care providers they
own generally have to continue drawing business from competing
insurers.
"Health plans want to exert pressure on provider systems, but
they don't have a product without providers in it, so they're
moving carefully," said Sam Glick, a partner with consulting firm
Oliver Wyman, a unit of Marsh & McLennan Cos.
UnitedHealthcare's new Harmony plan in the Los Angeles area is
built around Optum doctor groups, which supply all the primary-care
physicians. The insurer says premiums for Harmony cost roughly 20%
less than broader networks, and it is selling well.
But the company doesn't always have that many doctors in a
market. In San Diego, Harmony is using non-Optum doctor groups. As
Harmony potentially rolls out in other locations, including Texas
and Seattle, it may have a mix of Optum and non-Optum doctors, the
company said. Mr. Falkenberg said the Optum health-care providers
don't get special treatment from the insurer.
Many employers are skeptical of health plans with very limited
choices. A survey last year by the Kaiser Family Foundation found
that 39% of employers wouldn't reduce their network sizes for cost
savings. Another quarter said they'd need to see savings of at
least 30%, a high bar.
Individuals have shown more interest, through either the
Affordable Care Act exchanges or Medicare Advantage, said Gary
Claxton, a senior vice president at the Kaiser Family Foundation.
"They're making an individual choice of plan, and they're not
shopping for 5,000 different people in different places," he
said.
Aetna is adding free MinuteClinic visits without trimming its
networks, and it's unclear if the move will save money. A 2016
study in Health Affairs using Aetna data to look at 11 low-risk
health conditions found retail-clinic use was associated with
higher spending.
CVS Health pointed to an earlier study it funded that looked at
a broader array of health costs and tied retail-clinic use to lower
spending.
Troy Brennan, an executive vice president at CVS Health, said
the free MinuteClinic visits would benefit Aetna members and trim
costs. "Aetna is interested in making sure people get the best care
they can, in the most effective way possible," he said.
Write to Anna Wilde Mathews at anna.mathews@wsj.com
(END) Dow Jones Newswires
February 23, 2020 11:14 ET (16:14 GMT)
Copyright (c) 2020 Dow Jones & Company, Inc.
Grafico Azioni UnitedHealth (NYSE:UNH)
Storico
Da Mar 2024 a Apr 2024
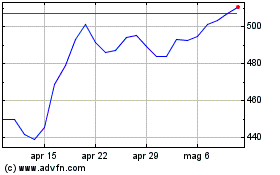
Grafico Azioni UnitedHealth (NYSE:UNH)
Storico
Da Apr 2023 a Apr 2024
